The coronavirus divide: Why five groups are dying more than they should
By Philip Whiteside, news reporter, and Carmen Aguilar Garcia, data journalist
Fourteenth century commentators writing about the Black Death told tales of the houses of the rich lying open for anyone to plunder, as both servants and their masters had died of the plague.
Death, it has been said since Roman times, is the Great Leveller.
Coronavirus – the closest the 21st century has come to a plague sweeping across the world – has not been a leveller, according to official data that has now been made available.
It has hit those on the margins and from disadvantaged communities the hardest.
It debunks claims by Michael Gove, made after Prime Minister Boris Johnson and Health Secretary Matt Hancock came down with the virus, that it “does not discriminate”.
Sky News analysis has found that COVID-19 has hit people in the UK in five main categories harder than others:
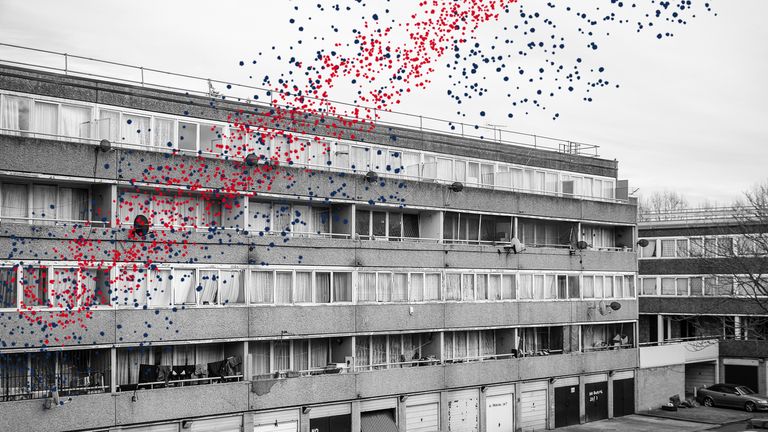
- People from deprived areas
- People in low-paid or low-skilled occupations
- The elderly
- People with underlying health conditions
- Those from black and ethnic minority communities
1. The deprived
People who live in deprived areas have generally shorter life spans, and are always hit harder by outbreaks of disease or seasonal illnesses.
But the difference between the most deprived and least deprived areas has been particularly stark because of COVID-19.
Between 1 March and 17 April, analysis shows there were 55.1 coronavirus-related deaths per 100,000 in the most deprived areas compared to 25.3 per 100,000 in the least deprived – more than double the rate.
Experts like David Finch, from the Health Foundation, say the link to deprivation is not surprising.
He told Sky News: “There are two key ways in which people can be affected by COVID-19.
“That’s first off through exposure and then how well people cope if they have the virus.
“If you look at people living in more deprived areas, they’re far more likely to have an existing health condition.
“We would see that as a consequence of the day-to-day conditions which they live in: That could be working long hours, variable shift patterns, and the stress that can be brought on through living in insecure housing.
“All that will have a toll on your underlying health.”
The Office for National Statistics’ (ONS) deprivation indices look at a range of inequalities, including levels of wealth, life expectancy, health, crime, employment and other “domains” which it uses to ranks areas from the most deprived to the least deprived.
In general, the most deprived areas of the country – based on the proportion of the bottom 10% sub areas in each local authority – are places like Middlesbrough, Liverpool, Knowsley and Hull.
Among the deprived areas that have been badly affected are: Newham, Lewisham, Haringey, Birmingham, Wolverhampton, Sandwell, Liverpool, and Middlesbrough – many of those that are the most deprived.
Naveed Sattar, professor of metabolic medicine at the University of Glasgow, says it is partly about the virus itself.
He said: “In the past, most viruses like pneumonia, and others that infected people, they didn’t have this effect on multi-organ systems.
“There’s something about this virus that affects more than just the lungs – for example, around a third get deep vein thrombosis, and others, even if they don’t get deep vein thrombosis… the blood thickens, which then affects the blood supply to your lungs, to your kidneys, to your heart, and also potentially the brain as well.
“So, if you’ve already got accelerated ageing because of obesity, smoking, poor lifestyle or accelerated age of your metabolism or your heart, if your organs are not as efficient to begin with, you’re much more likely to succumb.”
2. Lower paid, lower skilled occupations
The ONS found that people in lower-skilled, lower-paid jobs are more likely to die from COVID-19 than those in higher paid roles.
They are twice as likely to die with the virus than the average working man and four times more likely to die than those men in professional occupations.
Security guards, taxi drivers and chauffeurs, chefs, care workers and bus drivers are the male occupations with the highest death rates involving coronavirus.
Women working in care, leisure and services sectors are twice as likely to die as those in associate professional and technical occupations.
Experts say the degree to which people have been exposed – and significantly whether they have been using personal protective equipment (PPE) or other barriers if they are exposed – has become apparent.
Professor Keith Neal, emeritus professor of epidemiology of infectious diseases at the University of Nottingham, told Sky News: “Transport workers, particularly drivers of taxis, seem to be badly affected. And you can probably see why – if you’ve got different people in your cab all the time.
“Whether black cab drivers have been as badly affected, nobody quite knows. In the black cab, you often have a partition up, which you would expect to reduce the risk.
“The big surprise about the occupations wasn’t so much which ones were included, but which ones were not. Healthcare workers didn’t seem to be as affected as you might expect.
“It probably means what we’ve known for years – that proper use of PPE… is highly effective. PPE isn’t easy to use.”
The bus driver
Nadir Nur, 48, from Hackney, was a father of five. He drove the 394 from Islington to Homerton hospital in east London every day. In late March he caught coronavirus and later died. His son Joseph says:
At first, when we found out he wasn’t feeling very well, we didn’t really think much of it, because you don’t really think these things will hit you.
When it started getting worse, he was struggling to breathe, struggling to do anything.
He went into hospital, then into ICU. When it got confirmed, that’s when we really started fearing for the worst because he was mildly asthmatic.
He got put into a coma and about three, four days after that he developed a blood clot in his lungs and went into cardiac arrest. He died about one o’clock in the morning on 2 April.
Before he got sick, he was worried about it, but he wasn’t the sort of person who would hide away from anything. He had a job to do, and he would do it.
His route was to Homerton hospital. It goes through Hoxton and Hackney and then it stops there.
That’s probably part of the reason why – you’re passing the bus driver every time you get on the bus.
The response the government had – I think everyone agrees it’s quite poor – the protection they provided, the procedures that were in place.
If it was on the front of [politicians’] concerns, I think a lot more would have been done. It took a couple of people dying for them to look at it and realise.
He was a family man. He was there for everyone in the family – holding us all together, always arranging things, helping anyone in the family who needed it.
He looked after us all really well. He raised us into people I’m proud to say I am. He was just an amazing person.
It was just the biggest shock as I believed him to be the strongest person I know. Even when he was in the hospital, I was thinking ‘you’ll get through it’, because it was him.
3. The elderly
It was apparent from early on in the epidemic that elderly people were expected to be more likely to die.
Data out of China indicated that most deaths were occurring in older people – indeed much of the criticism of the government’s handling of care homes was due to it being well known early on that old people needed to be protected.
The findings from China and later Italy have been borne out in England and Wales too.
In England and Wales, overall, one person in 1,406 died and subsequently had coronavirus mentioned on the death certificate during the epidemic outbreak (weeks 12 to 21).
But this rose substantially for older age groups.
Among the over 90s, 1 in 59 died with COVID-19 during the eight weeks analysed compared to 1 in 198 of those aged 75 to 90 and 1 in 937 of those aged 65 to 74.
Prof Neal says it has been deaths in care homes that have been responsible.
He said: “The rate of infection among older people should be less, because they’re not going to work, so they’re less likely to catch it, but when they do catch it, it’s much worse.
“It’s been skewed by deaths in care homes. Very old people seem to be more likely to get it because they are in institutions.
“It’s almost impossible to keep it out because care home workers – you’re infectious before you get symptoms – go into work, asymptomatic, and introduce the infection. And that’s been all over Europe, not just a British problem.”
However, given that only people who have tested positive or are suspected to have had the virus and died had coronavirus recorded in their death certificates, a more accurate measure of the impact of the virus is excess mortality.
This is the additional deaths in a given period above what would have been expected under normal conditions.
Many of these extra deaths (other than those that would have been expected) have been caused by COVID-19, but there are other, as yet unexplained excess deaths that have also occurred in that period. It is likely that many of these have occurred as a consequence of the crisis and the lockdown – e.g. people not seeking treatment, or not being able to get treatment, for a potentially fatal condition.
The 82-year-old
Birnham Roberts, from the West Midlands town of Smethwick, had diabetes and had suffered a number of minor strokes. In March he caught coronavirus and died in hospital, where his daughter Cherelle believes he caught the virus. Before he was admitted with confusion, he was fit and active. Cherelle says:
He seemed a bit confused – muddling his words and not making much sense when he was talking.
He had a history, so, we brought him to the hospital hoping we could get him checked out, to see if he’d had another stroke.
The next day, they thought he had some sort of a chest infection. He was in a bay with lots of other people.
After two or three days, they said he had COVID.
They tried various antibiotics. Nothing seemed to be working. And then, you were just watching him fade away.
I got a call early in the hours of the morning. By the time I got there, he had passed. That was 18 March. It took nine days.
Normally, he was fit and well. He was still driving and active. He’d go to the gym, he’d do tai-chi… swimming most days. He was very active in the church – a church warden.
He’s got grandkids and he was very active with them as well.
[Before] I don’t think there was a lot of stuff out [about coronavirus] at the time. I remember I planned to go and see Cheltenham and they were thinking about cancelling it, but that’s all I remember.
What might have helped would have been putting out more accessible information, because with the older folk, they’re not really tech savvy, they’re not really going to be on the internet and finding things out that way. So, you probably need people to approach them. They’re not going to go out and seek the advice. Somebody would have to bring it to them.
It’s definitely something he would have picked up while he was in the hospital. I really regret taking him.
He was someone who was just always full of energy, always very community-minded, always helping out people.
He was in his 80s, but he would still go around and make sure that friends and members of the church were okay. He was always very caring about his community.
4. Underlying health conditions
As with the data on age, a Chinese study identified early on that people with some underlying health conditions were more likely to die from COVID-19.
In the same way that people in Britain with some occupations have been disproportionately hit by the outbreak, those with some chronic diseases and illnesses have also died to a greater extent than the rest of the population.
90.4% of the people who died with COVID-19 in England and Wales in March and April had at least one pre-existing condition, according to data from the ONS.
That figure includes deaths in care homes and the most common pre-existing condition was dementia and Alzheimer’s disease, which may be because the virus is more severe in older population groups.
Meanwhile, an analysis of NHS England data, which includes only deaths occurring in hospitals, shows that 95% of those who died in an English hospital up to 26 May had a pre-existing health condition.
While older people are more likely to suffer underlying health conditions, among younger people, the proportion who died who had a health issue was also high.
82% of those aged under 39 who died in English hospitals had a pre-existing condition.
Prof Sattar said part of the problem may be linked to obesity, as fat cells can make immune proteins which can contribute to a potentially fatal hyper-immune response. But, compounding the problem may be that underlying conditions make it harder for people’s bodies to cope if one occurs.
He said: “Males, poorer people, tend to be more overweight and obese and have more health conditions.
“Men compared to women tend to get cardiovascular disease and diabetes at younger ages so they’re more susceptible.
“There are groups… who by accelerated ageing of their cardiovascular and respiratory systems or age, have less of an ability to cope with the considerable stress that the immune response can cause on multiple organs in your body.
“Once you get a response, the ability to cope with that response is diminished, in the sense that their capacity – of their lungs, their hearts, their blood vessels, their metabolism – to cope with it is diminished.”
It all adds up to a finding that won’t surprise many – that COVID-19 was by far the biggest cause of death during the period.
The Asian cardiologist
Ajit Kumar Agarwal, 68, from a village near Bury St Edmunds, worked in hospitals in East Anglia and the United Arab Emirates. Two days after he retired, he came down with a fever. He died just under three weeks later. Nitika Agarwal, his daughter, says:
My dad had had a 45-year career.
He retired from full time work on Monday 23 March and fell ill on Wednesday 25th with a fever.
He was taken to the hospital on 1 April and then passed away two weeks later on 15 April.
He had Type 2 diabetes, but it was very well controlled on medication and he also had hypertension, which was controlled.
We thought it was very likely to be coronavirus, when he went into hospital, because he had been really feverish for a week.
At the time, people were talking about how the cough was really the thing to look out for – he didn’t have one, only a fever.
I don’t know what would have changed the outcome but he was encouraged to stay at home for quite a long time.
The virus has clearly done quite a lot of damage in the week he was at home. He deteriorated pretty quickly after getting to hospital.
We think it’s highly likely he picked it up seeing patients.
He was being very careful. Just before he retired, he was actually working in the UAE. He was telling us how he was disinfecting his keyboard and mouse and washing his hands.
It’s highly likely he would have mentioned something – so our assumption is that he was not wearing PPE at that stage.
It only really came out afterwards that diabetes was a significant risk factor.
I find it hard to believe that that wouldn’t have been picked up through the Italian or Chinese experience which preceded ours. Had that information been out there, I imagine some doctors who have those risk factors might have refrained from seeing patients, rightly so, and protected themselves more.
Information dissemination has been an issue.
He was completely and utterly dedicated to medicine, absolutely passionate about his job and had plans to bring cardiology to the community via GP practices – focusing on prevention at the primary care level.
He loved a good fancy dress party. A romantic at heart, he was a passionate poet. He used to write on scraps of envelopes and bits of paper, and he’d keep them all in a bundle. He’s got over 500 short couplets, and small poems and speeches he’s delivered for friends.
He was a real family person – happiest when he was with us. He has two grandchildren who are obviously completely devastated.
5. Ethnic background
Unlike for health issues and age, there was nothing in the early Chinese studies that identified ethnic background as a risk factor.
Yet, it has become apparent that people from a black and minority ethnic (BAME) background are significantly more at risk of dying from COVID-19 than white people.
It is under investigation but is already controversial – with some commentators linking it to the poorer conditions in which BAME people live, because of systemic racism in society.
The ONS says geographic and the socio-economic factors (such as deprivation, household composition, disability, age, among others) account for over half of the difference in risk between males and females of black and white ethnicity.
However, these factors “do not explain all of the difference, suggesting that other causes are still to be identified,” the ONS analysis adds.
The experts say the causes, while still under investigation and awaiting further research, are complex.
Seif Shaheen, professor of respiratory epidemiology at Queen Mary University, London, told Sky News he had just set up a new study to try to examine some of the reasons that may not be spotted by the ONS.
He said: “The link is undisputed both in the UK and in the USA. There’s quite a long list of possible explanations for that.
“One is that, in this country, South Asians and Afro-Caribbeans have more in the way of comorbidities, such as diabetes, heart disease and hypertension.
“Also higher levels of deprivation. They may live in poorer housing.
“And specifically… if you take South Asians, in particular, they live in extended families, multi-generation families, and therefore they live in very overcrowded homes.
“This is a very contagious infectious virus. If you’re in a very overcrowded home, you’re more likely to catch it, and also more likely to get a bigger dose of the virus, which may mean that you then get the illness more severely.
“And being in the BAME community… they’re more likely to be in either patient-facing occupations – in health care or social care – in public-facing jobs, for example, working on public transport. Therefore, they are more exposed… to the infection because they come into contact with people more.”
His comments are borne out by other ONS data
The ONS found that the greatest rate of COVID-19 deaths was among people aged 20-64 in low skilled elementary occupations and in caring, leisure and other service occupations.
Other ONS data shows black workers are one and a half times as likely as white workers to be in “elementary” jobs – jobs like labourers, cleaners and package deliverers and twice as likely to be in caring, leisure and other service jobs.
Pakistanis and Bangladeshis, according to the ONS, are more than twice as likely to work in sales and customer service roles than white people and nearly three times as likely to be plant and machine operatives. Both those fields had a much higher than average rate of death from COVID-19.
But Prof Shaheen said there could be other, less obvious reasons, why BAME people are being so badly affected.
He said a colleague called Adrian Martineau had found, through randomised trials, that vitamin D deficiency may make people more susceptible to respiratory infections, of which COVID-19 is a type.
He added: “People who are dark-skinned are more likely, particularly in the UK and in a temperate climate, to be vitamin D deficient.”
In addition, he continued: “Smoking is probably important. Some sub groups in the BAME community, Bangladeshi men particularly, smoke an awful lot.
“At the moment, there’s a heck of a lot we don’t know.”
Another expert said much of the medical evidence does not take other factors into account.
Dr Manish Pareek, associate clinical professor in infectious diseases at the department of respiratory sciences, University of Leicester, works on a COVID-19 ward but has also done work in the community with tuberculosis.
He and a group of colleagues have been looking at the impact of culture and ways of living on the spread of coronavirus. He also views household size and occupation as important.
But, he added: “The other thing that we haven’t really got any idea about, is, if you think about how the public health messaging has been set out by the government. It’s been very much centrally driven by the five o’clock press briefings that Boris or others do. What we don’t know is whether people from different ethnic groups really listen to those public health messages.
“I work in Leicester. We are approximately 40% foreign born. The government’s public health messaging, which is adverts, Twitter, maybe Facebook and in the bus shelters… I’m not sure those are the ways that they receive that information.
“More likely is that they receive their information from their relatives or friends through WhatsApp messages from overseas, different news channels. They don’t necessary watch Sky…
“All of those things mean… I’m not sure how well the messages got through.”
What can or should be done?
The experts Sky spoke to were adamant that more work was needed in order to understand what had caused the divide the ONS has identified. But, also, that more needs to be done to address some of the causes that are already apparent.
Prof Pareek said: “There’s likely to be a second wave or certainly some spikes in the next few months. Who knows when? And therefore, it’s important that we try and tease this information out now, when things are a bit quieter.
“So we can put those public health messages out and be quite clear that we know that if you’re of black ethnicity or, say, Bangladeshi ethnicity, your risk of death and being infected is quite high, you need to do X, Y and Z.
“It’s not just ethnic minorities, it’s going to be also those who are deprived and those with underlying health conditions. But those groups are slightly different, because if you had an underlying health condition, you were put under shielding. I’ve not seen anything relating to any of that for the ethnic minority population.
“If you’re a bus driver, in their late 60s say, coming up to retirement the next year or two, and we know that you’ve got diabetes etc, it may not make sense to me that they should be seeing hundreds of people.
“If you look at the medics who’ve died, some of them probably shouldn’t have been on the frontline.
“If we know that these groups are at higher risk, how are we going to target those higher risk populations with vaccination programmes? We already know that in certain ethnic minorities groups, vaccination coverage is lower. We should proactively be thinking about this.”
Prof Shaheen agreed: “If you sort of run through the checklist of risk factors, obviously, a lot of them can’t be changed. You can’t change your ethnicity. You can’t change the diseases you’ve got. So it comes down to probably a limited number of modifiable risk factors linked to lifestyle.
“The other thing would be that it’s important those in patient-facing and public-facing occupations are sufficiently well protected, which comes back to the whole PPE debate. Many in those sort of jobs – other than those in the very front line, ICU and so on – often feel that perhaps they haven’t had adequate protection.”
The Health Foundation, meanwhile, believes what’s needed is a wider rethink about how people from deprived communities are treated.
David Finch added: “From a longer-term perspective, there’s certainly a case that you could see more of a preventative approach in the health system – trying to keep healthy people healthy, so they don’t need to rely on the health care system.
“There was a kind of thrust from government around taking a preventative approach. That’s something that’s important to prioritise in future so that we can be keeping people healthy and not relying on the NHS to step in when people become ill.”
Source: Read Full Article