Inside ‘overloaded’ Barnet Hospital where ambulances wait hours to drop off patients
Outside Barnet Hospital the ambulances stack up and patients such as Ray Newell wait in the vehicles because there simply isn’t space inside.
“I’ve been waiting about an hour,” says Ray, who has damaged his coccyx in a fall. “It is frustrating because I want to go in there.”
Kneeling beside him is nurse Rebecca Borne who says she too is frustrated: “Yesterday was very busy; 42 people waiting for beds in A&E, which means people like poor Raymond here get stuck outside and we have to treat people in the ambulance.”
“It’s not fair – he’s in a lot of pain and all we’ve got are gas and air for him.”
Members of staff say ambulances have had to wait up to three hours in recent days. The target time is to offload patients within fifteen minutes.
This is a worrying bottleneck – not just for patients waiting in the back – but if the ambulances can’t offload, they are not available for further call-outs.
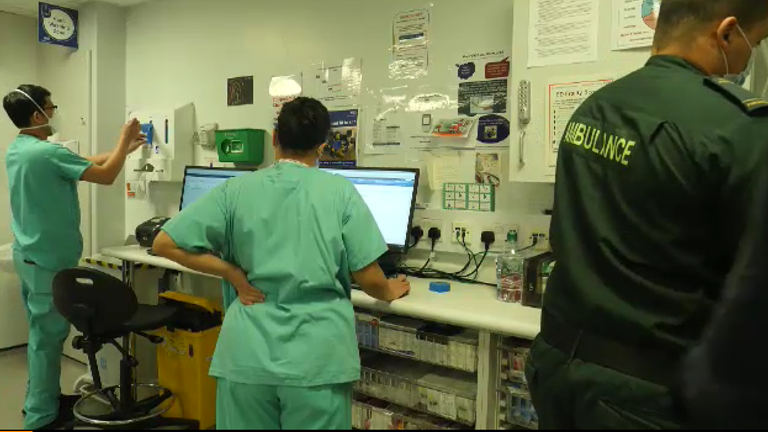
Also, sometimes the ambulance paramedics are coming into the hospital with patients – because there are not enough staff to look after them.
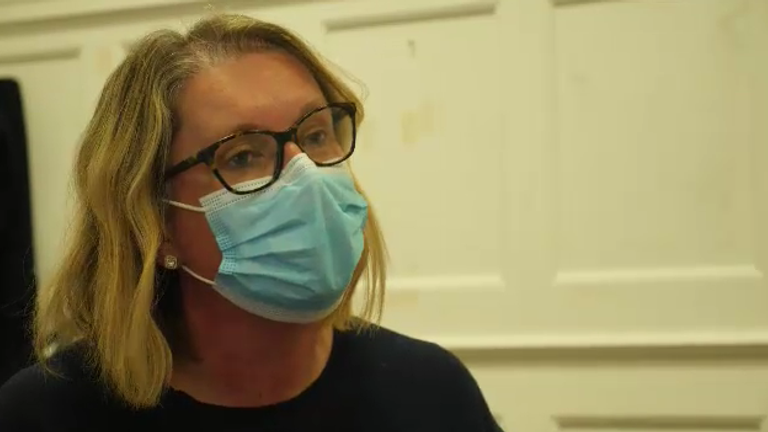
“We are full up to the front door,” says Sarah Stanley, divisional medical director at Barnet Hospital.
Harrowing reality of a coronavirus ward – where exhausted medics fight to keep patients alive and some don’t make it
“You might have five or six ambulances waiting 60 minutes or longer and cumulatively that time across London is ginormous.
“The worry is around the uncertain risk of that patient who has dialled 999 and that ambulance cannot get to them in a timely way.”
Sarah has just come off a call with the other London regions and they are all experiencing similar problems.
One plan they’ve agreed is called “rapid release” which has never been used before in London.
If there is a “seven-minute call” such as a cardiac arrest – the patient waiting outside hospital will be left with the emergency department – even if they don’t have room – to allow the ambulance back into the system.
So, then the consideration is how to create bed space. Sarah says, for example, she has some elderly homeless patients who she could release, but with the temperatures so cold right now, can she be sure they would find a shelter?
On the geriatric ward, patients might be well enough to leave but local care home staff are isolating with COVID, and don’t have the resources to take them back.
On some wards, there are spare beds but because one person tested positive, the whole ward is sealed off and the remaining patients have to isolate – even if they were due to be discharged.
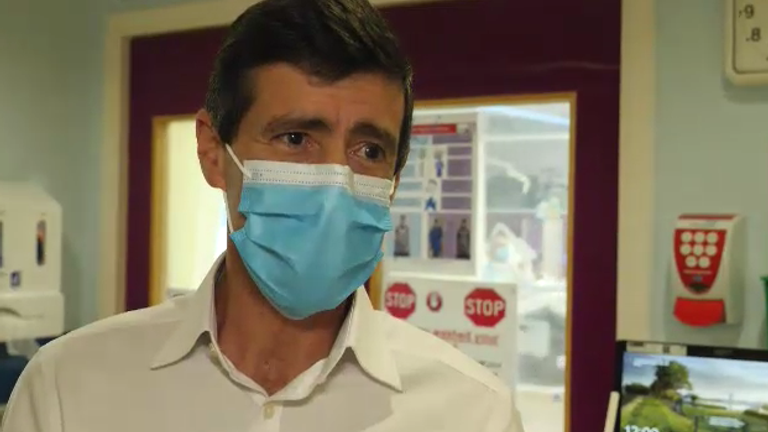
Consultant geriatrician, Dr David Levy, explains: “What it means is this bay is now shut, probably for two weeks while we wait for the remaining patients to go through a period of isolation.”
“We can’t admit any new patients into this bay until it is cleared and cleaned…”
So, in order to free up space, the hospital is getting creative. Adult Assessment Unit, next to A&E, is adapting into a makeshift ward to create more space, overseen by the matron, Karen Kirwilliam.
Fuelled by an early morning espresso and armed with a smile behind her mask she calls up the site team to get nine extra blow-up mattresses for the patients.
“We’ve got a huge demand for beds at the moment and it’s hard. The staff have been absolutely incredible. They’ve gone above and beyond anything we could have asked for.
“When you’re watching the media and they are saying this is a war, we don’t have soldiers – but we do have NHS staff and they are our superheroes.”
It turns out the army is being brought in to help in London hospitals, but as yet, none are assigned to Barnet.
In the emergency department, two consultants discuss the staff shortages. Dr Erik Witt tells his colleague: “We’ve had another doctor call in sick. We’re haemorrhaging doctors. So next week we are down to three out of seven.”
“That’s tight!”, replies Dr Russell Durkin.
He tells me: “The department is overloaded with patients. We’ve had no exit flow to the wards upstairs.
“Over the last few days, we’ve had waits of up to 8-9 hours to see a doctor, especially at night time.”
Alan Swedloff, 77, has been admitted with a heart condition. He should be on a ward but after 20 hours he’s still in A&E.
While praising the NHS staff he is critical of people who’ve not been vaccinated for taking up space.
“What they don’t understand is it isn’t just a case of protecting themselves – they are being selfish because they are taking up beds that need not be taken up. And that is putting more pressure on the health service.”
On the COVID wards at Barnet, they say a few months ago they had many serious unvaccinated young people with the delta variant – now they are seeing more elderly vaccinated people with Omicron.
Omicron symptoms seem milder, but unvaccinated COVID patient, 38-year-old Julea Ali, who contracted the illness at a Christmas party says she nearly died.
“I’m just catching my breath back,” she says having just walked a few paces to her chair.
She’d twice booked and then cancelled her vaccination after reading misinformation about the dangers of the vaccine online.
“All the social media controversy kind of made me think is it right or is it wrong? So, I will now obviously be doing the vaccination. It is the biggest regret. I should have listened to my family and friends.
“When I was at home, when the ambulance came up, I was on my last breath and my oxygen was below 70, so I was quite close to death.”
There are far fewer people dying of COVID than there were when I visited the hospital this month a year ago.
Back then staff faced high death rates and they were fighting an illness they were still learning about. But everyone I spoke to in the hospital says this year is harder.
They still have COVID patients, but they also have a growing backlog of much-needed operations, and a greater number of people are presenting with other complications in A&E than they did last year.
On top of that, this system, which relies on teamwork – is too many team members down.
Source: Read Full Article