COVID-19: How will Pfizer vaccine be rolled out to GP surgeries?
The Pfizer/BioNTech COVID-19 vaccine is set to be rolled out to GP surgeries within days.
From Tuesday, people will be able to receive the vaccine at GP practices, a week after the first approved vaccines were administered in hospitals across the UK.
Sky News spoke to the chair of the Royal College of General Practitioners (RCGP), Professor Martin Marshall, about how that will happen and who will get the vaccine initially.
Who will get the vaccine and how will they know they have been chosen?
People aged 80 and over will be the first to get the vaccine in GP surgeries.
Prof Marshall said: “You’ll receive an invitation if you’re in that priority group.
“Please don’t call up the surgery to get a vaccine or turn up, wait to be called.”
He said there will be “some flexibility” at a local level to prioritise the more vulnerable within that age group, such as certain ethnicities or people with multiple conditions.
What will the procedure be once a person gets to the surgery for their vaccine?
Like getting a flu jab, people will have to arrive at the surgery on time and check-in with the receptionist.
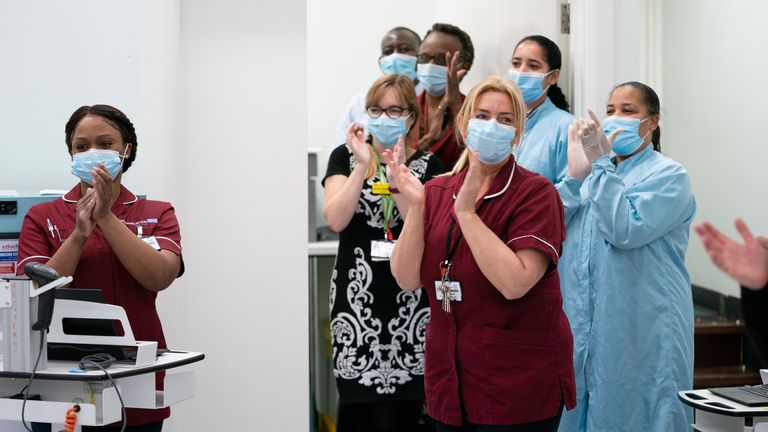
“Staff will be in necessary PPE and you will be lined up with appropriate social distancing,” Prof Marshall said.
“There will be staff at every stage of the process, and they will describe the risks and get the person’s consent.”
Staff, most likely nurses, will take a vial out of the fridge and mix it with saline solution, ready to be used.
Then, the vaccine will be injected into the person’s arm and they will have to wait in another part of the surgery for 15 minutes.
What are the risks and is it safe to have the vaccine in a GP surgery?
Because two NHS staff had reactions to the vaccine on the first day of the roll-out, everybody has to wait for 15 minutes before they can leave the surgery.
Anybody with a history of anaphylaxis to medicines or food should not be invited to have the vaccine.
The risk is low, but if anybody does suffer anaphylaxis, GP surgeries are well equipped to deal with it.
“GPs don’t have the immediate support of a hospital but they have basic life support, oxygen, Piriton – all things that will treat anaphylaxis quickly and safely,” Prof Marshall said.
Will all GP surgeries be giving the vaccine?
No. Practices will be chosen by Public Health England (PHE) to become vaccine hubs on the basis they will stay open for longer to ensure all the vaccines they have can be used.
Will the chosen GP surgeries still provide a normal service?
Not every staff member in a surgery will be part of the vaccine programme, but PHE has told chosen practices to prioritise the vaccine.
Patients might be able to get advice over the phone, but Prof Marshall said if they need “more detailed or urgent care” then they can go to a nearby practice.
This is the busiest time of the year for the NHS, and on top of the vaccine, they will continue to deliver the flu vaccine and treat patients.
“Practices will help each other out, we’re all in this together,” he said.
“It’ll show the NHS at its best.”
The vaccine needs to be stored at -70C, how will GP surgeries cope with that?
Prof Marshall explained that the vials, which contain five doses each, will be transferred from PHE’s main freezers to hospitals across the UK that have -70C freezers.
“The vaccine can only be moved three times so once it’s in the hospital freezer it has to be delivered from there to 200-250 odd GPs around the country that have been chosen,” he said.
“When they receive a pack – 975 vaccines in one box – they’ll be put into a fridge in the practice, they’ll thaw and then they have five days to use them all.
“This isn’t going to be perfect, certainly not from day one and mistakes will be made, but I hope not too many.
“We have such a strong record of delivering mass vaccinations, I’m very confident general practice can do this well.
“GP staff are so well trained that I hope mistakes will be minimal and we’ll learn very quickly.”
Will people in care homes be given the Pfizer vaccine?
They will, but because the logistics are even more difficult than getting it to GP surgeries, the medicines regulator, the MHRA, is still deciding how best to do that.
Prof Marshall said it will not be for the first week, but when the rollout is approved either a GP or a practice nurse will go into a care home and administer the vaccine.
Subscribe to the Daily podcast on Apple Podcasts, Google Podcasts, Spotify, Spreaker
“The biggest risk of taking them out of the centres into people’s homes is denaturing the vaccine or wasting it,” he said.
“We need to be cautious before we take that risk.”
Source: Read Full Article