Coronavirus: Surgeons wear full PPE in six-hour cancer operations during pandemic
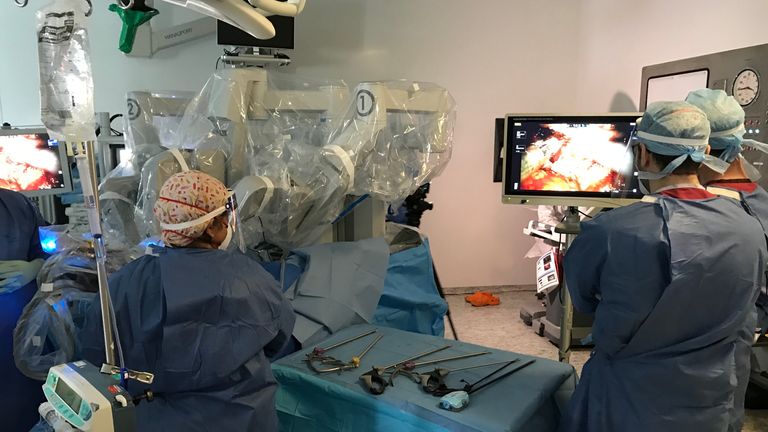
At first glance everything looked normal in the operating theatre.
Centre stage was a large surgical robot, its arms deep inside a heavily draped patient.
In the far corner, the consultant surgeon used a 3D console to control the instruments that were snipping away at the man’s prostate cancer. An anaesthetist and a couple of theatre staff completed the cast.
It was a carefully choreographed scene I had seen many times in almost two decades as a health correspondent.
Only this time everyone was wearing full PPE. Respiratory masks, visors, and two pairs of gloves securely sealed to a disposable gown.
The staff assume all patients are positive – even when they test negative – and they take no risks.
It’s hot and uncomfortable to wear – and I wore it for barely an hour. Imagine a six-hour operation. But it’s worth it.
A new study has tracked 500 cancer patients who have had surgery at University College Hospital in London, during the peak of the pandemic. Just 10 were diagnosed with COVID-19 in the weeks that followed – and none died.
That’s a big deal. Research from Wuhan showed one in five patients died following surgery if they had coronavirus. That’s because surgery interferes with the immune system.
And cancer would have increased the risks still further.
But the success isn’t just down to the PPE.
The building is separate to the main University College Hospital site with its busy A&E that takes all-comers. Only cancer patients who test negative for the virus are admitted. Staff also undergo regular tests.
And even if the virus does make it past the front door, clinical rooms are ventilated between patients and the operating theatres are deep cleaned between procedures.
I watched the operation with Professor John Kelly, who led the team at the hospital.
He told me: “The risk is real. We do not know who comes in with COVID. Despite having the PPE, with all the risks we are minimising this is functioning really well.”
Many cancer services have been suspended during the pandemic because the risk of coming into hospital was thought to be too high for vulnerable patients. But there is now a backlog of thousands of operations, and delays in treatment can cost lives.
I spoked to Dr Veeru Kasivisvanathan, the lead author of the research, in the recovery area just as the first patients were coming out of surgery.
He said it was important the NHS found a way of operating on high-risk patients because a second wave of the virus is highly likely.
“If you reduce the chances of COVID entering into hospital you can continue high volume cancer surgery with good outcomes for patients, which is particularly important because we know globally two million operations are cancelled every week. Hopefully others can learn from what we have done.”
The key test is whether patients are confident enough in the safety measures to come to hospital.
Source: Read Full Article