Why opioids are such an American problem
When it comes to taking opioids, the United States has the dubious honour of leading the world.
For every one million Americans, almost 50,000 doses of opioids are taken every day. That’s four times the rate in the UK.
There are often good reasons for taking opioids. Cancer patients use them for pain relief, as do patients recovering from surgery (codeine and morphine are opioids, for example).
But take too many and you have a problem. And America certainly has a problem.
In two years, the town of Kermit in West Virginia received almost nine million opioid pills, according to a congressional committee.
Just 400 people live in Kermit.
Nationally, opioids killed more than 33,000 people in 2015, according to the Centers for Disease Control and Prevention.
That figure includes deaths from heroin, an illegal opioid. But almost half involved a prescription opioid – that is, a painkiller available from a pharmacy with a note from a doctor.
So why does America – more than any country in the world – have an opioid problem?
There is more than one cause. But these are some of the most important.
American doctors prescribe – a lot
Unlike most European countries, the US does not have universal healthcare paid for by taxes.
Instead, Americans must get their own insurance – usually via an employer or the government.
“Most insurance, especially for poor people, won’t pay for anything but a pill,” says Professor Judith Feinberg from the West Virginia University School of Medicine.
“Say you have a patient that’s 45 years old. They have lower back pain, you examine them, they have a muscle spasm.
“Really the best thing is physical therapy, but no one will pay for that. So doctors get very ready to pull out the prescription pad.
“Even if the insurance covers physical therapy, you probably need prior authorisation (from the insurer) – which is a lot of time and paperwork.”
The CDC says opioid prescriptions have fallen by 18% from their peak in 2010. But the total is still three times higher than in 1999.
‘I saw this drug on TV’
The US and New Zealand are the only countries that allow prescription drugs to be advertised on television.
According to the research firm Kantar, spending on advertising by pharmaceutical companies in the US reached $6.4 billion in 2016 – a rise of 64% since 2012.
None of the 10 most-advertised brands in 2016 was an opioid. But mass-marketing of drugs has an effect, says Professor Feinberg.
“As a clinician, people will come and say ‘I saw this on TV – can you give me this drug’.
“Sometimes they were so confused, they were already on the drug – they were using the brand name, where I used the generic name.”
In 2015, the American Medical Association called for a ban on adverts for prescription drugs. It didn’t happen.
Three months later, the extent of America’s opioid culture was seen at half-time of the Superbowl – the country’s most expensive advertising slot.
A 60-second ad was devoted to opioid-induced constipation. The advert – paid for by AstraZeneca – advised sufferers to visit their doctor and “ask about prescription treatment options”.
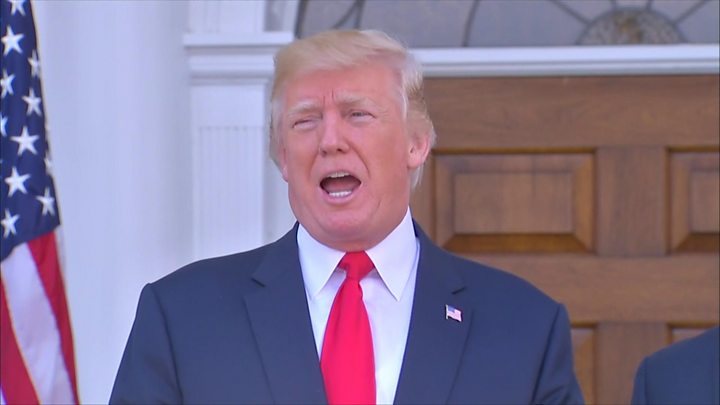
President Obama’s chief of staff was not impressed.
Gifts to doctors
In the US, it is common for drug companies to court doctors, in an effort to promote their products.
“When you’re a doctor in the US, these detailing people (salespeople) come in from the industry,” says Professor Keith Humphreys from Stanford University.
“They are invariably smooth, friendly, attractive, sharply dressed, adorable, they’re giving out gifts to everybody. They host dinners, they sponsor conferences, they sponsor junkets.
“That is going to affect prescribing.”
For the past four years, the US government has published the amounts paid by drug and device companies to doctors and teaching hospitals.
The total in 2016 was more than $8bn. More than 630,000 physicians had payment records.
For example, Purdue Pharma – which makes OxyContin, a popular opioid painkiller – made almost 80,000 transactions in 2016, worth more than $7m in total.
In 2016, a study looked at the link between doctors, the free meals they received from drug companies, and the medication they prescribed.
The study found receiving free meals was “associated with an increased rate of prescribing the promoted brand-name medication”.
Pharmaceutical companies say their reps are merely sharing information with doctors. But Professor Humphreys says there is a “corrupting” influence.
“We need a pharma industry, it’s not that it’s wrong,” he says. “But you can’t let the fox guard the hen house.
“I would create completely clear blue water between the people that manufacture drugs and all the training and operation of the healthcare system.”
Pharmaceutical companies also spend money on health care workers and organisations in other countries.
In the UK in 2016, companies gave £116m ($153m) to health workers and organisations for non-research and development in 2016.
But, although the UK figure is 7% higher than in 2015, it is less than 2% of the amount paid in the US.
Poor training
Dr Richard Frank is professor of health economics at Harvard Business School, and served in the Health Department from 2009 to 2016, during President Obama’s administration.
He thinks medical training in the US has not been good enough.
“Physicians have received almost no training in pain management,” he says.
“Until recently they have been under some pretty important misconceptions about how addictive various products are.”
He adds: “A couple of years ago I testified before congress when I was in government. One of the representatives, before going into congress, was a thoracic surgeon.
“He noted that he had gotten almost no training in pain management – and what he had learned came entirely from the nursing staff he worked with.”
Dr Frank says medical training isn’t the only reason for America’s opioid problem. “There’s plenty of blame to go round,” he says.
But his criticism is echoed by Professor Judith Feinberg.
“Doctors didn’t learn anything about addiction at medical school,” she says.
“That is now changing, but everyone who’s a doctor already, didn’t learn anything. I learned about opioid drugs in the part of pharmacology where we learned about anaesthesia.
“Probably the whole topic of anaesthesia-like drugs was two hours. People don’t have much knowledge about opioids. There was no curriculum that includes addiction.”
Bad science?
In 1980, Dr Hershel Jick wrote a short letter to the New England Journal of Medicine.
It said that “despite widespread use of narcotic drugs in hospitals, the development of addiction is rare in medical patients with no history of addiction”.
The claim has been debunked, and the letter now carries an online warning note. But Dr Jick’s letter had a big impact.
This year, Canadian researchers said the letter had been cited 600 times – usually to claim opioids weren’t addictive.
In the late 1990s the Veterans Health Administration – which runs healthcare for military veterans – pushed for pain to be recognised as the “fifth vital sign”.
This gave pain equal status with blood pressure, heart rate, respiratory rate, and temperature.
Then in 2001, the Joint Commission – which certifies almost 21,000 US health organisations and programmes – established standards for pain assessment and treatment.
In 2016, the JC released a statement that claimed that “everyone is looking for someone to blame” for the opioid problem. It insisted that its 2001 standards did not “require the use of drugs to manage a patient’s pain”.
But Professor Feinberg says the VHA and JC’s moves meant doctors were under pressure to prescribe strong painkillers – such as opioids – when they may not have been necessary.
“By the time you reach middle age, it’s a rare person who doesn’t ache somewhere,” she says.
She adds that – in a country where patients rate their doctors, and low ratings can affect doctors’ earnings – the score can be influenced by whether patients receive opioids.
A culture of medication
Some Americans, says Professor Keith Humphreys from Stanford University, believe that life is “fixable”.
“I’m 51,” he says. “If I go to an American doctor and say ‘Hey – I ran the marathon I used to run when I was 30, now I’m all sore, fix me’, my doctor will probably try to fix me.
“If you do that in France the doctor would say ‘It’s life, have a glass of wine – what do you want from me?'”
In 2016, a study compared how Japanese and American doctors prescribed opioids. It found that Japanese doctors treated acute pain with opioids in 47% of cases – compared to 97% in the US.
“There is obviously a willingness, and a habit, of giving opioid pain relief that is not shared elsewhere,” says Professor Feinberg.
“Other countries deal with pain in much healthier ways.”
Get our morning briefing direct to your inbox, each weekday morning
Source: Read Full Article