New Pandemic Plight: Hospitals Are Running Out of Vaccines
As the coronavirus tears across much of Texas, Dr. Esmaeil Porsa is grappling with one of the most formidable challenges he has faced: The Houston hospital system he operates is running out of vaccines.
Dr. Porsa, the chief executive of Harris Health System, which treats thousands of mostly uninsured patients, warned on Friday that its entire vaccine supply could be depleted by midday Saturday. The problem is not one of capability — the vaccination centers Dr. Porsa oversees have easily been administering as many as 2,000 vaccines a day — but of availability.
“All of a sudden the distribution of vaccines stopped,” Dr. Porsa said. “It’s perplexing and frustrating because I keep hearing that there are high percentages of vaccines that have been distributed but not administered.”
In the midst of one of the deadliest phases of the pandemic in the United States, health officials in Texas and around the country are growing desperate, unable to get clear answers as to why the long-anticipated vaccines are suddenly in short supply. Inoculation sites are canceling thousands of appointments in one state after another as the nation’s vaccines roll out through a bewildering patchwork of distribution networks, with local officials uncertain about what supplies they will have in hand.
In South Carolina, one hospital in the city of Beaufort had to cancel 6,000 vaccine appointments after it received only 450 of the doses it expected. In Hawaii, a Maui hospital canceled 5,000 first-dose appointments and put 15,000 additional requests for appointments on hold.
In San Francisco, the public health department had at one point expected to run out of vaccines this week because the city’s allocation dropped sharply from a week ago and California officials temporarily had to put thousands of doses on hold after a higher than usual number of possible allergic reactions were reported. In New York State, officials in Erie County have canceled thousands of vaccine appointments in recent days after a sharp decline in allocations from the state.
The situation is especially dire in Texas, which is averaging about 20,000 new coronavirus cases a day, fueling concerns over whether officials will be able to curb the spread when they cannot get their hands on the vaccines they desperately need to do so.
Health officials trying to piece together why this is happening are puzzled by reports that millions of available doses are going unused. As of Friday morning, nearly 39.9 million doses of the Pfizer-BioNTech and Moderna vaccines had been distributed to state and local governments, but only about 19.1 million doses had been administered to patients, according to the Centers for Disease Control and Prevention.
Pfizer and Moderna have each agreed to provide the United States with 100 million vaccine doses, and the companies are racing to manufacture the vaccines, together releasing between 12 million and 18 million doses a week.
At that rate, it is feasible for the Biden administration to meet the president’s pledge to inject 100 million vaccines by his 100th day in office. Public health officials could even potentially ramp up the pace of vaccinations with existing supply.
It appears that problems with distributing the already available doses are responsible for many of the acute vaccine shortages now being seen in parts of the country. Factor in the ever-increasing demand as more states make the vaccine widely available to those 65 and older, and officials warn that distribution headaches could persist in the weeks ahead.
The Biden administration has pledged to overhaul distribution to the states and even use the Defense Production Act to increase supply, but vaccine experts warn that shortages of the doses will persist in the short term with manufacturing sites already facing capacity constraints.
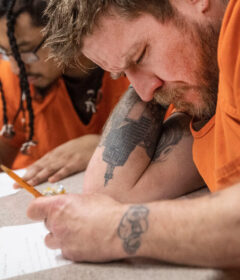
State and local governments, as well as hospital administrators, are fending for themselves. In Houston, Dr. Porsa said his staff was scrambling as the supply of vaccines dwindled this week, squeezing six doses out of vials intended to provide five.
In one sign of the confusion around vaccine distribution in Texas, officials in Dallas County scrapped a plan this week that would have prioritized shots for people living in heavily Black and Latino communities hit hardest by the virus. Texas state officials threatened to slash allocations of the vaccine if the county went ahead with the plan even though data showed that most of the shots administered in Dallas County had been in wealthier neighborhoods.
Houston, the fourth-largest city in the country, is now struggling with a similar problem as the hospitals serving some of its poorest residents run out of the vaccine, prompting some public health experts to question why doses are not being made more available to vulnerable communities.
Covid-19 Vaccines ›
Answers to Your Vaccine Questions
While the exact order of vaccine recipients may vary by state, most will likely put medical workers and residents of long-term care facilities first. If you want to understand how this decision is getting made, this article will help.
Life will return to normal only when society as a whole gains enough protection against the coronavirus. Once countries authorize a vaccine, they’ll only be able to vaccinate a few percent of their citizens at most in the first couple months. The unvaccinated majority will still remain vulnerable to getting infected. A growing number of coronavirus vaccines are showing robust protection against becoming sick. But it’s also possible for people to spread the virus without even knowing they’re infected because they experience only mild symptoms or none at all. Scientists don’t yet know if the vaccines also block the transmission of the coronavirus. So for the time being, even vaccinated people will need to wear masks, avoid indoor crowds, and so on. Once enough people get vaccinated, it will become very difficult for the coronavirus to find vulnerable people to infect. Depending on how quickly we as a society achieve that goal, life might start approaching something like normal by the fall 2021.
Yes, but not forever. The two vaccines that will potentially get authorized this month clearly protect people from getting sick with Covid-19. But the clinical trials that delivered these results were not designed to determine whether vaccinated people could still spread the coronavirus without developing symptoms. That remains a possibility. We know that people who are naturally infected by the coronavirus can spread it while they’re not experiencing any cough or other symptoms. Researchers will be intensely studying this question as the vaccines roll out. In the meantime, even vaccinated people will need to think of themselves as possible spreaders.
The Pfizer and BioNTech vaccine is delivered as a shot in the arm, like other typical vaccines. The injection won’t be any different from ones you’ve gotten before. Tens of thousands of people have already received the vaccines, and none of them have reported any serious health problems. But some of them have felt short-lived discomfort, including aches and flu-like symptoms that typically last a day. It’s possible that people may need to plan to take a day off work or school after the second shot. While these experiences aren’t pleasant, they are a good sign: they are the result of your own immune system encountering the vaccine and mounting a potent response that will provide long-lasting immunity.
No. The vaccines from Moderna and Pfizer use a genetic molecule to prime the immune system. That molecule, known as mRNA, is eventually destroyed by the body. The mRNA is packaged in an oily bubble that can fuse to a cell, allowing the molecule to slip in. The cell uses the mRNA to make proteins from the coronavirus, which can stimulate the immune system. At any moment, each of our cells may contain hundreds of thousands of mRNA molecules, which they produce in order to make proteins of their own. Once those proteins are made, our cells then shred the mRNA with special enzymes. The mRNA molecules our cells make can only survive a matter of minutes. The mRNA in vaccines is engineered to withstand the cell’s enzymes a bit longer, so that the cells can make extra virus proteins and prompt a stronger immune response. But the mRNA can only last for a few days at most before they are destroyed.
“These are our frontline workers who are at the greatest risk of contracting the virus and at the greatest risk of spreading it to others,” said Vivian Ho, a health economist at Rice University and Baylor College of Medicine. “We would be able to resolve the pandemic in Harris County quicker if we could get a sufficient number of vaccines,” she added, referring to the county encompassing much of Houston.
Adding to the turmoil, just days after Gov. Greg Abbott of Texas, a Republican, praised the state’s vaccine rollout at a meeting in Houston where Democratic city and county officials were excluded from participating, the lieutenant governor, Dan Patrick, also a Republican, sent a letter on Thursday to the state’s Expert Vaccination Allocation Panel urging its members to fix the problems.
“Right now, in many cities and counties when an announcement of available vaccinations is made, website sign-up pages crash and phone calls go unanswered,” Mr. Patrick said in the letter. “Texans need to have a better understanding of the time it will take for everyone to be vaccinated in order to reduce lines, confusion and frustration.”
The sense of chaos afflicting the distribution efforts, not just in Texas but in an array of states, is laying bare how local officials are struggling to fill the void left by the lack, until this week, of a comprehensive response at the federal level.
Dr. George Rutherford, an epidemiologist at the University of California, San Francisco, said the most obvious problem with vaccine administration in the San Francisco area was clear: “There’s not enough doses, period,” he said. “That’s it. Everything would work fine if you had enough doses.”
The public health department in San Francisco and hospitals in the city were “caught by surprise” by the lack of doses, Dr. Rutherford said, and by the eligibility expansion to those 65 and older, which likely strained the system. Varying vaccine distribution channels — such as Kaiser Permanente and the University of California, San Francisco — receive the doses on their own, he said, further complicating an already convoluted distribution system.
“So it’s a little hard for the city to understand exactly what’s left over, what they need to do, where the holes are to fill,” Dr. Rutherford said. Still, new vaccination sites are opening in San Francisco, which Dr. Rutherford said would help speed the process along once more doses become available. “There’s this tension between efficiency and equity,” he said. “It’s never easy.”
Dr. Grant Colfax, head of the San Francisco Department of Public Health, said the city was “very close to doses running out,” and said a lack of overall coordination has led to distribution problems.
“I think what this really is, is a continuation of the fallout of the lack of a coordinated federal response,” he said. “Basically cities and counties were left on our own to deal with this pandemic.”
He said local jurisdictions “simply did not have the resources and the capacity” to handle the complicated effort without help. “It has manifested in a very tragic way.”
In Austin, Texas, Curt Fisher, a 76-year-old who has served on the boards of several high-tech start-ups, experienced firsthand the confounding roadblocks to securing a vaccine. He was playing golf with friends several weeks ago when they learned that Austin Public Health had vaccines available.
They quickly registered with their cellphones from the golf course and landed appointments in a matter of minutes. The system was swiftly deluged and Mr. Fisher, who had waited about 30 minutes to call, missed out.
He doggedly checked the website from his home, about four or five times a day, for more than three weeks. Each attempt bore the same result: no vaccines available within the maximum 100-mile search radius.
Then after days of pinning his hopes on his hometown health service, good fortune finally came from more than 150 miles away. He received a text from a Memorial Hermann hospital in Houston, where he was automatically registered because he had seen a doctor about three months earlier, inviting him to come to the hospital for his first dose of the vaccine.
He made the roughly three-hour drive on Monday, spending about an hour at the hospital with little waiting for his first shot of the vaccine. He is supposed to go back on Feb. 8 for the second and final injection. Looking back, Mr. Fisher said the success he found in Houston and the hassles he went through in Austin illustrated that some vaccine distribution centers “really have their act together” and others do not.
“I don’t think the system that Austin Health had could handle the stress of the high volume, obviously,” he said.
But some people have struggled to get vaccine appointments, only to see them canceled because of supply problems.
Jeanelle Fernandes, 33, who has sickle cell anemia and lives in Miami, initially felt relieved after setting up a vaccine appointment for Jan. 28.
Having it confirmed “was kind of like a light at the end of the tunnel,” she said. “This has been a really hard journey for me.”
But then Baptist Health South Florida tweeted this week that all first-dose vaccine appointments scheduled for Jan. 20 or later would be canceled. “I’m definitely frustrated,” she said. It was not the hospital’s fault, she said; she blamed a government that seemed unprepared to roll out millions of vaccine doses when people urgently needed them.
“Now, I have to wait,” Ms. Fernandes said. “I’m up in the air, I don’t know what’s going to happen.”
Katie Thomas and David Montgomery contributed reporting.
Source: Read Full Article