Inside the Medical Examiner’s Office, Where Opioids Fuel Surge in Deaths
In the operations center of the Office of the Chief Medical Examiner on a recent Wednesday, a large dashboard showed that 39 people had died unexpectedly across the city — at home, or accidentally, or violently — over the last 24 hours. That was more than on Sunday, but fewer than the 45 deaths on Monday, almost always the office’s busiest day of the week.
Four years ago, numbers that high would have been a disturbing aberration in the city’s regular pulse of life and death. Today, they are the “new normal,” says Dr. Jason Graham, New York City’s chief medical examiner.
“We were anticipating that as the pandemic waned, our cases would fall back to sort of a prepandemic equilibrium, but they really haven’t,” he said.
Since 2018, homicides are up. People are dying from health issues that went unaddressed in the pandemic, as well as from Covid-19, and, probably, the still uncertain long-term health effects of the disease. But by far the largest factor in the increased work at the medical examiner’s office — which investigates all the city’s sudden, unusual and suspicious deaths — is a sustained jump in accidental drug overdoses, mostly from the opioid fentanyl.
There were nearly 2,700 drug overdose deaths in the city in 2021, the highest total in at least two decades, and 2022’s official toll is expected to be even higher. On average, the city has a fatal drug overdose death every three hours. While official numbers are still pending, Dr. Graham said, December 2022 will most likely be the worst single month on record.
Every overdose victim in the city ends up at the medical examiner, where samples of tissues and blood are carefully extracted, then distilled into glass vials and stacked into trays dozens deep. Long after the bodies are released to family members, toxicologists do the work of figuring out exactly what killed them.
“If not for the pandemic, this would be the public health emergency of our lifetimes,” Dr. Graham said.
For the scientists who work at the medical examiner’s office, analyzing the constant stream of death can be grueling. It comes after the office, the city’s mortuary, handled an unimaginable number of fatalities in the early waves of Covid-19, transporting and storing some 31,000 bodies in 2020 and 2021, with disaster morgues, freezer trucks and all staff pressed into service to help.
Now, victims can be found with needles still in their arms, a once-rare phenomenon that is a sign of how quickly fentanyl can kill, Dr. Graham said. Family members sometimes say they didn’t know to intervene, because they mistook the labored breathing of an overdose for snoring.
Fentanyl Overdoses: What to Know
Devastating losses. Drug overdose deaths, largely caused by the synthetic opioid drug fentanyl, reached record highs in the United States in 2021. Here’s what you should know to keep your loved ones safe:
Understand fentanyl’s effects. Fentanyl is a potent and fast-acting drug, two qualities that also make it highly addictive. A small quantity goes a long way, so it’s easy to suffer an overdose. With fentanyl, there is only a short window of time to intervene and save a person’s life during an overdose.
Stick to licensed pharmacies. Prescription drugs sold online or by unlicensed dealers marketed as OxyContin, Vicodin and Xanax are often laced with fentanyl. Only take pills that were prescribed by your doctor and came from a licensed pharmacy.
Talk to your loved ones. The best way to prevent fentanyl use is to educate your loved ones, including teens, about it. Explain what fentanyl is and that it can be found in pills bought online or from friends. Aim to establish an ongoing dialogue in short spurts rather than one long, formal conversation.
Learn how to spot an overdose. When someone overdoses from fentanyl, breathing slows and their skin often turns a bluish hue. If you think someone is overdosing, call 911 right away. If you’re concerned that a loved one could be exposed to fentanyl, you may want to buy naloxone, a medicine that can rapidly reverse an opioid overdose and is often available at local pharmacies without prescription.
Justine Pardi, one of the lab’s toxicologists, said she copes by focusing on the work and “not thinking about the case behind every single sample you’re doing, because that would just be overwhelming.”
Her boss, Gail Cooper, the head forensic toxicologist, reminds her staff that their work brings closure to families. It also helps police decipher what is in the drug supply, shapes health policy and provides information to the public about why street drugs have become so deadly, even for people who just use them occasionally.
To keep up morale, staff members decorate their meeting room with cotton snowballs in the winter and flowers in the spring. In a flash of gallows humor, they taped a sign on their huge walk-in refrigerator door showing the actor Christopher Walken’s face.
“This fridge is the Walken fridge,” it says.
But the decorations cannot mask the smell of formaldehyde, or the rows of jars and vials connected to a person who died of a suspected drug overdose. There are thousands of people represented in the refrigerator and freezer behind it, their bodily fluids stored near the extracted contents of their stomachs and tiny slices of their brains and livers.
Perhaps more than anywhere else in the city, here is where you can get a visceral sense of the enormousness of the opioid epidemic’s toll.
Forensic scientists by necessity must have a hard shell, but the scale of death they have faced in the last few years has sometimes astonished them. “I’ve been in this field now for over 20 years, and I have never seen anything like this,” Dr. Cooper said.
Increasingly, taking illegal drugs is the highest-risk activity for New York City residents. Drug overdoses used to account for around 60 percent of all accidental deaths in the city — a category including pedestrians struck by automobiles, industrial accidents and falls. Now, they account for between 80 and 85 percent, Dr. Graham said.
Fentanyl, a synthetic opioid that can be 50 times stronger than morphine, is mixed into both the city’s heroin and its cocaine supplies and is involved in 80 percent of its accidental overdoses. The patterns reflect national trends: Deaths from drug overdoses rose nationally to record-breaking levels in 2021, nearing 108,000, according to the Centers for Disease Control and Prevention.
In some of the most publicized recent cases, fentanyl-laced heroin took the life of the actor Michael K. Williams in his Brooklyn apartment in September 2021. Two months later, the same combination killed the 10-month old daughter of Daniel Auster, the son of the author Paul Auster; Daniel himself died of an overdose in 2022 after being charged in his daughter’s death.
Fentanyl-laced cocaine can be particularly deadly, sometimes killing several users with the same batch. In March 2021, for example, a trading executive, a first-year lawyer and a social worker died separately after ordering tainted cocaine from the same illicit delivery service. Each case came through the medical examiner labs, whose work helped in criminal prosecutions.
“The message has to get out that if you’re coming to the city to party for the weekend, and you go to the club and just want to pick up some cocaine, you are going to get fentanyl,” Dr. Graham said.
The Opioid Crisis
From powerful pharmaceuticals to illegally made synthetics, opioids are fueling a deadly drug crisis in America.
The toxicology lab is catching up from a backlog that began in early 2020, when the first wave of Covid-19 shut the lab for several months. It takes about 60 days to get a toxicology result, down from more than 90 last year. The office is getting extra staff, and four new machines arrived in mid-February to speed up the processing of blood and tissue extracts, much to Dr. Cooper’s relief.
“It feels like Christmas,” she said.
From the vials, the toxicologists see patterns emerging months or years before they make it into headlines. Along with an array of fentanyl analogues, they note a rise of xylazine, a powerful veterinary tranquilizer that was once only seen in the deaths of people with access to veterinarian’s offices. There’s also an increase in designer benzos, meant to mimic drugs like Xanax, mirroring a trend in Europe. And there is a growing trickle of a little-known class of illicit opioids known as nitazenes.
“You’re constantly having to look for the next thing,” Dr. Cooper said. “We are always feeling like we’re chasing them.”
Some other jurisdictions have stopped doing autopsies on every drug overdose because of the volume, along with a national shortage of medical examiners. But the city’s medical examiner’s office still analyzes each case. It now performs close to 7,000 autopsies a year, up from just over 5,000 in 2018.
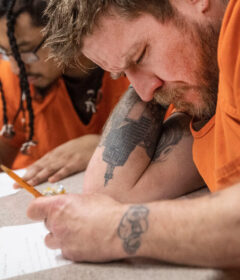
Overdose deaths have hit Black men in their 50s and 60s particularly hard, as well as the city’s homeless population. At least 815 homeless New Yorkers died in public spaces, shelters and hospitals during the 2022 fiscal year, the most on record, according to city data. Almost 600 of those deaths wound up in the medical examiner’s office, which ruled 330 of them overdoses.
With the number of deaths rising, the medical examiner’s office is hiring a team of social workers, funded in part by the city’s millions in opioid settlement funds, with the goal of reaching family members of each fatal overdose victim.
The task stretches the boundaries of what people think of as the job of a medical examiner, but investigators say that in their on-the-scene dealings with grieving family and roommates, they are finding needs no other city agency is addressing.
The social workers have no agenda but simply express condolences and ask if the people connected to the deceased need help themselves. In most of the 80 cases it has handled since the program began in September, someone has said yes, said Hannah Johnson, the new program’s manager.
People have asked for help in applying for emergency rent assistance, in navigating Surrogate’s Court, in finding a therapist and in accessing naloxone to stop another opioid death. They have asked about what fentanyl is or about how long the grief will last. But often, they just want someone to listen, said Kate Sutherland, one of the two social workers who has been making the calls.
“Somebody literally said to me last week, ‘It’s so nice to know that somebody there is seeing my daughter as a person and not as another case,’” Ms. Sutherland said. “That just goes such a long way for somebody.”
Source: Read Full Article