Beneath a Covid Vaccine Debacle, 30 Years of Government Culpability
Washington has rejected plans to revamp vaccine preparedness for decades and repeatedly paid a price. The Biden administration is at a similar crossroads.
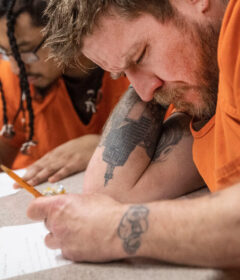
A vaccination site in Los Angeles in January. Credit…Bing Guan/Bloomberg
Supported by
By Chris Hamby and Sheryl Gay Stolberg
WASHINGTON — As the Biden administration tries to stanch yet another wave of the coronavirus pandemic, senior White House officials have also been considering a proposal to ensure the nation is better prepared for the next infectious disease outbreak.
Key to the plan is the creation of a taxpayer-funded “vaccine hub” where experienced drug makers would partner with the government, reliably churning out millions of doses under federal oversight.
The proposal is partly a response to a searing failure by a once obscure Maryland biotech firm, Emergent BioSolutions. While Pfizer and Moderna had spectacular success producing vaccines, the government entrusted the manufacturing of two of the other leading candidates to Emergent, which was forced to toss tens of millions of doses of Johnson & Johnson’s vaccine and to quit producing the AstraZeneca vaccine because of serious quality problems that ultimately led the Biden administration to cancel its contract.
The government’s partnership with Emergent, which cost taxpayers hundreds of millions of dollars over the past decade, was supposed to be a pillar of the nation’s pandemic preparedness. Instead, it proved to be the culmination of 30 years of frustrations.
Three times over the past three decades, presidential administrations explored plans for a vaccine overhaul like the one President Biden is now considering, only to be thwarted by pharmaceutical lobbying, political jockeying and cost concerns, a New York Times investigation found.
In each case, the nation was left ill prepared for the next crisis — while creating a vacuum that Emergent eagerly filled.
“The reason why Emergent got so many contracts is mostly because they were the only ones willing to do the work,” said Dr. Kenneth Bernard, a top biodefense adviser to Presidents Bill Clinton and George W. Bush.
To reconstruct the forgotten history that led to this year’s vaccine debacle, The Times reviewed thousands of pages of records — among them files from presidential and military archives, previously undisclosed government reports, industry correspondence and business plans.
Reporters also interviewed more than 30 people who have helped shape U.S. biodefense policy, including officials from five presidential administrations, corporate executives and industry consultants.
Time and again, The Times found, analyses commissioned by the federal government arrived at a similar conclusion: Ensuring access to specialized vaccines is a public good that cannot be left entirely to the market; yet it is unrealistic for the government to take on the task alone.
But while the government has tried to enlist major pharmaceutical companies, they have largely been reluctant to divert resources from commercial products. At the same time, they have stood in the way when the government has proposed its own factory, fearing a taxpayer-backed competitor.
Repeatedly, The Times found, a middle path won support in Washington: a government plant run by a major drugmaker. Budgets were drawn up and sites selected. In one case, the pre-eminent vaccine company Merck got on board.
But the momentum always evaporated. The government opted for incremental changes, dangling incentives before less experienced companies — chief among them Emergent.
Once again, a public health crisis has laid bare the heavy cost of that approach.
Purchases in past years of Emergent’s anthrax vaccine severely strained the budget of the nation’s Strategic National Stockpile, crowding out investments in products like masks that were in critically short supply last year, as The Times reported in March.
And as the government banked on Emergent to make both Johnson & Johnson’s and AstraZeneca’s Covid-19 vaccines, problems in Baltimore delayed immunization efforts around the globe. Nearly two years into the pandemic, the Baltimore plant has still not received final clearance from the Food and Drug Administration.
An Emergent spokesman, Matt Hartwig, acknowledged the company’s struggles but said it had taken on a difficult task that others would not.
“While everything has not always gone exactly as planned, we have remained steadfast in our commitment to the American people,” Mr. Hartwig said in a statement.
He noted that regulators ultimately authorized the release of 100 million Covid-19 vaccine doses made at the Baltimore site, with more still under review. Mr. Hartwig said the decision to end the federal contract was mutual. But a senior administration official said the government had stopped paying Emergent after discovering quality problems and later reached an agreement to terminate the partnership without a costly legal fight.
Now, as President Biden considers a future less dependent on Emergent, the experience of his predecessors provides both a road map and a warning.
The pandemic tested the current approach, said Dr. W. Craig Vanderwagen, who ran the federal office charged with preparing for health emergencies from 2007 to 2009 and is a business partner of Emergent’s founder.
“It was pretty clear that we failed.”
‘Over and Over Again’
Long before Operation Warp Speed, there was Project Badger.
Then, as now, the government scrambled to secure manufacturing capacity in the midst of a crisis, finding itself with effective vaccines but few places to mass-produce them. Then, as now, officials proposed greater federal intervention to ensure the nation wasn’t again caught unprepared.
In 1990, as the U.S. military planned an operation to expel the invading Iraqi army from Kuwait, officials received a sobering intelligence report: Saddam Hussein was probably in possession of anthrax and botulinum toxin.
The Defense Department had vaccines for both threats, but the supply was small. Project Badger searched for a solution.
Officials identified over a dozen companies that might be able to make more of the vaccines and tried to persuade them to help. None of them agreed, unclassified documents show.
The companies had concerns about legal liability and did not want to invest in switching production lines if the government couldn’t promise large purchases after the crisis. One company said that “the cost in lost business alone would have been $62M,” according to an Army memo.
Ultimately, the military had to limit vaccination to troops considered at the highest risk. Chastened, the Pentagon commissioned a study that recommended a federal site run by an experienced manufacturer. The government had embraced the model previously for weapons plants and Energy Department labs.
Source: Read Full Article